Recent studies have provided methods to detect infants and young children with cerebral palsy (CP) early. For infants who are high-risk, such as those born very premature, there are international guidelines to detect CP early using a range of sophisticated assessment tools (magnetic resonance imaging, General Movements Assessment using videos, standardized neurodevelopmental assessments). These tools are being used in Neonatal Follow-up programs that follow high-risk newborns systematically over the first years of life.
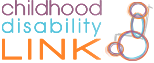
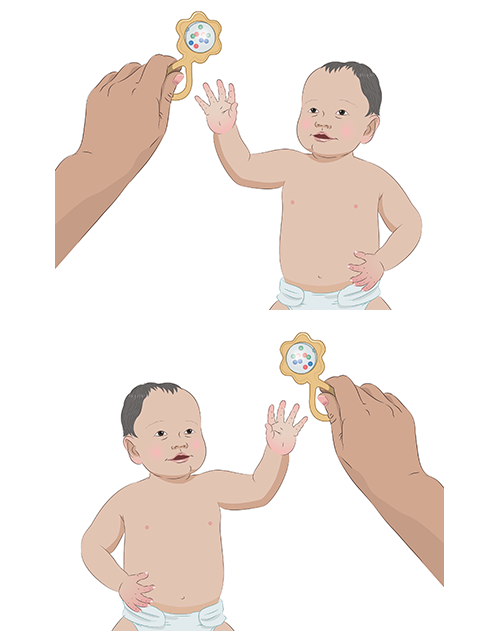
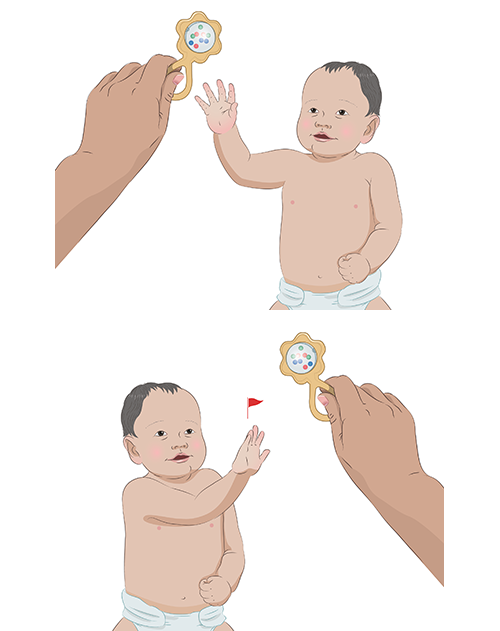
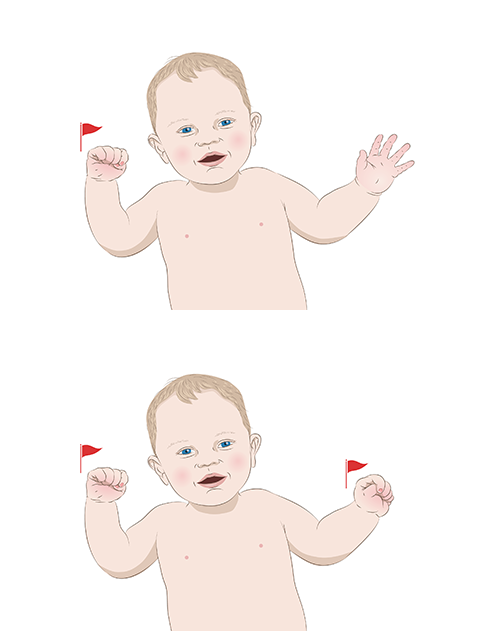
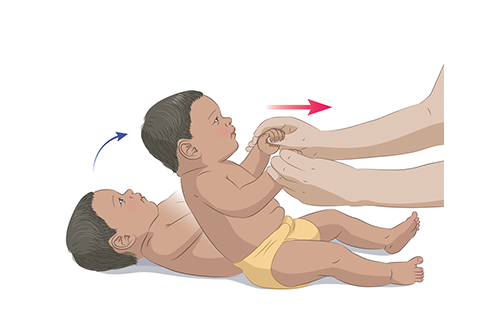
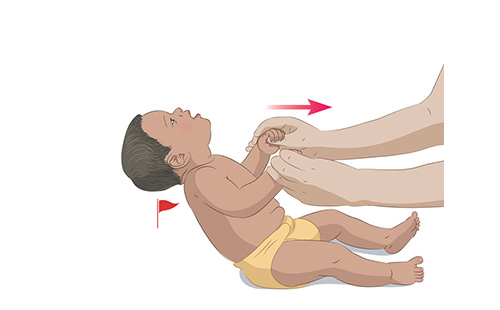
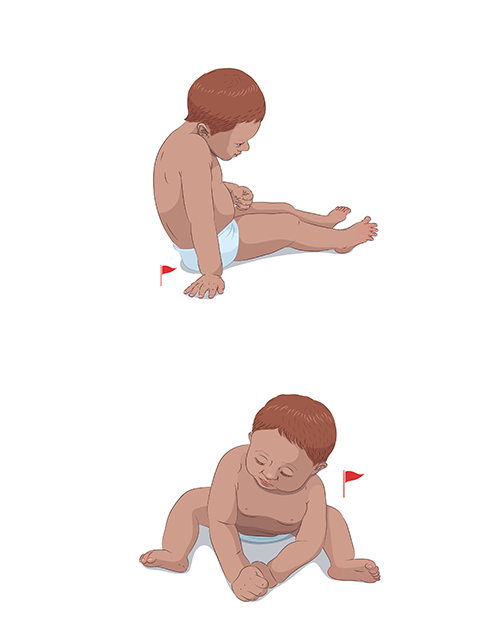
Many children with CP are not born early and did not have a high-risk delivery. A different strategy is needed for these children so that we can diagnose CP early. We developed a toolkit to help community physicians detect CP in infants as part of their well-baby care visits.